New antimicrobials on the way…
Posted:
August 11, 2017
Concerns about antimicrobial resistance have been growing for many years. At one point it seemed as though we were out of options -organisms were becoming resistant to all antibiotics on the market and no new drugs were being produced. A healthy return on investment for an antibiotic was lacking. The cost to develop a new drug is currently over $1 billion. Bacteria would become resistant and make the drug obsolete and all that investment would be a waste of money. But what were clinicians going to use for a sick patient when nothing on the market would be effective?

An attempt at a solution came in 2016 when the Obama administration created the Presidential Advisory on Combating Antibiotic-Resistant Bacteria (PACCARB) in response to Executive Order 13676. The fight against antibiotic resistant bacteria became a National priority. The objectives were as follows:
1. First, the unnecessary use of antibiotics was slowed with the implementation of antibiotic stewardship programs.
2. Second, surveillance efficiency and response to detection were brought to a national level with the creation of regional and national public health networks where antibiotic use and resistance data is shared quickly. International collaboration, surveillance, and control were also improved.
3. Third, Government funding was increased in order to facilitate and accelerate the development process of rapid detection and characterization devices, as well as support basic and applied research for the development of new antibiotics, other therapeutics, and vaccines.
Tax dollars were put to good use in our opinion. Since the implementation of the above-mentioned actions, the healthcare market has seen a few new antibacterial compounds make it to market. Some of the most promising ones are combinations of older compounds mixed with novel inhibitors – just give that old rice some extra spice! For example, two products to gain clearance recently are Zerbaxa (ceftolozane/tazobactam) and AvyCaz (ceftazidime/avibactam).
As for the state of our current pipeline, within the next three years, we should see from eight to twelve new antibiotics released to the market.
Great! We’ve given physicians the tools they need to save their patients! Unfortunately, just getting the antibiotics into a physician’s hands doesn’t completely solve the problem. Physicians rely on the microbiology lab to let them know which antibiotic will work against the organism causing disease. The microbiology lab needs a reliable AST (Antimicrobial Susceptibility Test) method in order to obtain that information.
In the past, the AST device manufacturers had to wait until the compound was cleared for use in humans before they could develop and submit the device for clearance. Thankfully, this process is changing. There has been a very recent push for pharmaceutical companies, device manufacturers, and the different branches of the FDA to jointly bring AST devices to market as close as possible to the time that the antibiotic itself is available for use. This way the antibiotic can be brought to the market and be used as effectively without delay as it was intended to.

Unfortunately, the current administration has proposed deep cuts for the 2018 Fiscal Year. The programs crucial in combating antimicrobial resistance initiatives such as CDC, Biomedical Advanced Research and Development Authority (BARDA), NIH, and United States Agency for International Development (USAID) are likely to be affected. While most programs will continue, uncertainties regarding the extent and scope of these programs persist, due to unknown funding levels at present.
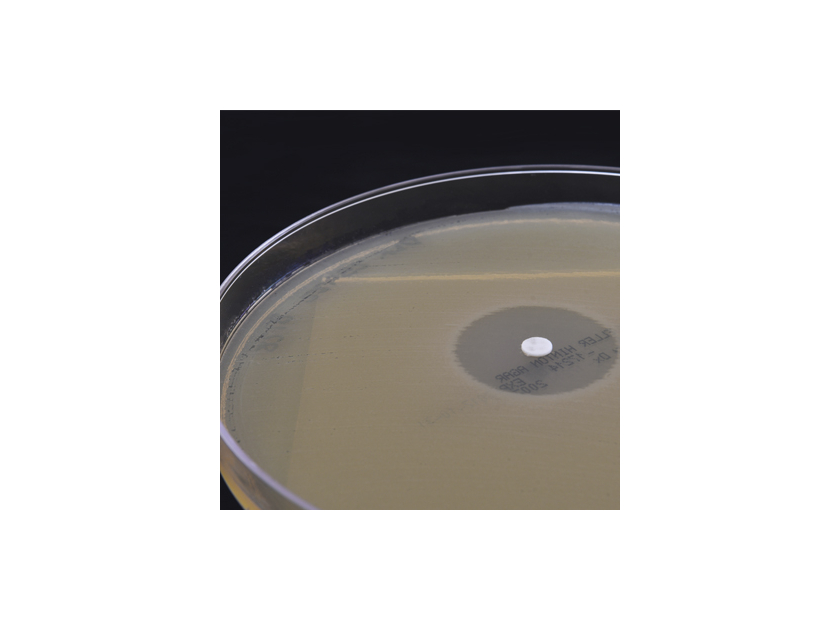
Most importantly, Hardy Diagnostics understands the importance of making AST devices available as quickly as possible. This is why we have a dedicated team that collaborates with pharmaceutical companies and the FDA to get HardyDisks™ available to laboratories as quickly as possible. Understandably, while Disk Diffusion is an older method dating back to the 1950s, it is still a wonderful tool and a staple in laboratories that many microbiologists still employ on daily basis and utilize for the confirmation of other methodologies, whenever needed. If read and interpreted carefully (i.e, slight enhancements when key indicator disks are placed strategically by each other, blunting of the inhibition zones, or even comparison of differences of zones between antibiotics of the same class) disk diffusion can provide valuable information.
After all, susceptibility results are crucial for patient care, and we at Hardy Diagnostics are proud of our history of consistently being the first manufacturer to provide FDA-cleared commercially available disks of new antibiotic compounds for the clinical community in the United States.
The authors, Andre Hsiung and Rianna Malherbe, head up the Hardy Diagnostics antibiotic disk development program.
Comment(s)