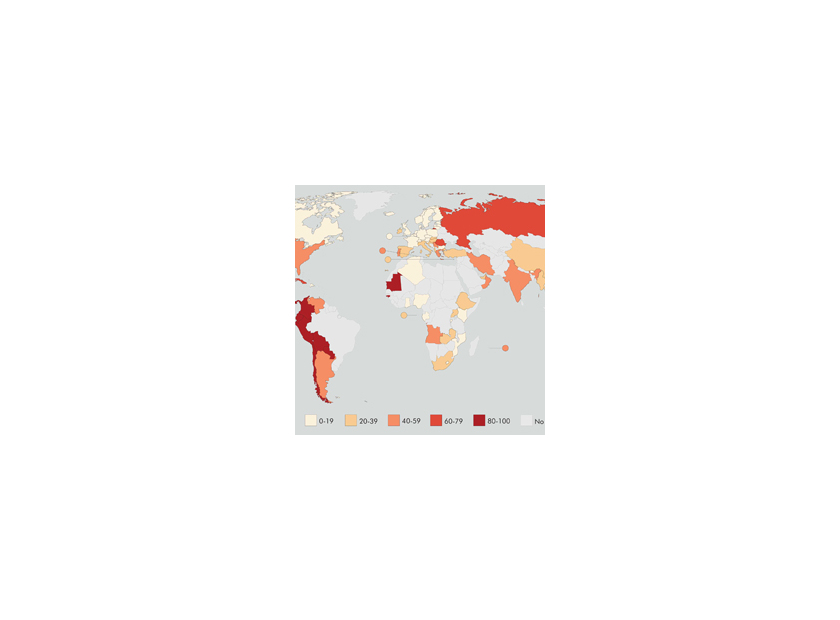
From 2002 to 2014, the rate of antibiotic-resistant infections doubled from 5.2% to 11% while the overall rate of bacterial infections has remained relatively constant (13.5 million to 14.3 million). Treating an antibiotic-susceptible infection costs an average of $1,394, while an antibiotic-resistant infection costs an average of $3,698.
There were approximately 1.5 million cases of antibiotic-resistant infections in 2014 and the additional cost of treating antibiotic-resistant infections totaled over two billion dollars (1). Antibiotic overuse, misuse, or misapplication has led to a selection of bacteria that have resistance to these drugs. As a result, cases of multi-drug resistant pathogens are becoming more common.
The Centers for Disease Prevention and Control (CDC) has identified bacteria from the Enterobacteriaceae family (enterics) and several other Gram-negative pathogens as a growing concern for antibiotic resistance (2). Many of these pathogenic enterics have acquired resistance to most of the commonly used antibiotics. Carbapenem-resistant Enterobacteriaceae (CRE), Pseudomonas aeruginosa, and Acinetobacter baumanii are of great concern because carbapenems are among the last-resort antibiotics for infections by these organisms3. Data obtained by the CDC indicates poor outcomes and high mortality (18-48%) for infections caused by CRE(3). Along with the increasing prevalence of these organisms, the economic burden and cost for hospitals is expected to rise even further. Carbapenem-resistant bacterial infections are a public health concern and could become an economic burden for hospitals and patients receiving treatment for these infections if the spread of these bacteria is not monitored or controlled.
In clinical settings, initiatives should be taken to follow an antibiotic stewardship program (ASP) in order to reduce overall costs and improve patient treatment outcomes. The CDC estimates that 30-50% of all antibiotics prescribed in the U.S. are unnecessary or inappropriate
(4). To help prevent the spread of antibiotic-resistant bacteria, the CDC encourages hospitals to implement ASPs. These programs are designed to optimize treatment and prevent the use of antimicrobials in an ineffective manner, such as for infections that are caused by a microorganism that is unaffected by the prescribed drug.
It has been reported that hospitals that implement ASPs have seen an increase in patient cure-rates through correct diagnosis, reduced rates of nosocomial infections, and reduced costs (4).
Some pathogens acquire antibiotic resistance in the environment or among animals, which in turn can infect human populations (5). Eighty percent of all antibiotics produced are being given to farm animals. The broad use of antibiotics in livestock feed is a public health concern since the resistant bacteria have been tracked from animal populations to humans by the National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS) (5). While non-pathogenic organisms are regular inhabitants of human and animal guts, other enterics with resistance traits will survive when antibiotics are administered.

The antibiotic-resistant enterics can be carried asymptomatically in the intestines of livestock and shed in feces. They are then spread to humans directly by contaminated meat and poultry products, or indirectly through the environment. Currently, however, the FDA has prohibited the addition of cephalosporins and fluoroquinolones to animal feed due to the overlap of these drug classes with human medicine.
In the arms race between humans and bacteria, some strains of bacteria have countered every new antimicrobial agent thrown at them and continue to evolve rapidly while new drugs are developed. This is not only a health problem but also an economic problem because as the prevalence of infections caused by antibiotic-resistant bacteria is increasing, so is the cost of patient care. Longer hospitalization stays, surgery, lost wages and productivity due to illness, and future complications caused by antibiotic-resistant bacteria are some of the additional factors that lead to the increased cost associated with these infections.
While the development of new antibiotics may not be the main focal point for the pharmaceutical industry, new agents have been launched recently (i.e. ceftolozane/tazobactam, ceftazidime/avibactam, meropenem/vaborbactam, and delafloxacin) and many newer antimicrobial candidates are in the pipeline between now and 2022.
However, there is still hope. Besides traditional antimicrobials, there are a variety of newer options that have yet to be fully explored, such as phage therapy and lytic enzymes (6). Although selective pressures and evolution by point mutations may be favoring the bacteria, cumulative efforts to practice antibiotic stewardship by industry and hospitals that utilize antimicrobials can help curb the rise of antibiotic-resistant pathogens.
References