The Nipah Virus...
Another Emerging Virus With a Very High Mortality Rate
Originates from bats
The Nipah virus (NiV) is a zoonotic virus of the genus Henipavirus, family Paramyxoviridae, and has been identified as a biosafety level-4 pathogen with a 40-75% fatality rate. The virus was first discovered in 1999 following a Malaysian outbreak among pig farmers which resulted in nearly 300 human cases and more than 100 deaths.(1) Given the virus’ genetic relation to Hendra virus, a rare bat-borne zoonotic disease, the fruit bat (genus Pteropus) was quickly identified as the host reservoir of NiV. This puts many South and Southeast Asian countries at risk for potential outbreaks.
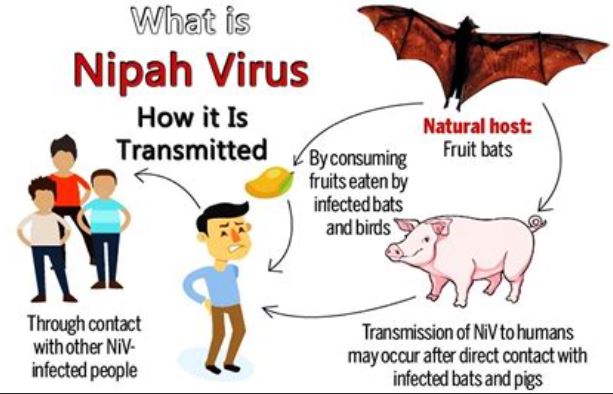
Humans are mainly exposed to NiV from infected fruit bats that pass the virus to farm animals. In countries like Bangladesh and India, consumption of fruit that has been contaminated with fruit bat urine or saliva has also been a main source of infection. Direct human to human transmission is also possible, usually with healthcare workers and family members of the infected. The symptoms of NiV infection in humans ranges from asymptomatic to acute respiratory infection or fatal encephalitis. Signs of NiV can include labored breathing, fever, cough, and headache. Severe cases can usually lead to seizures, which can progress to a coma within 24 to 48 hours.(2) The nonspecific initial symptoms of NiV make it difficult for accurate diagnosis and control measures. During the acute phase of the disease, real time polymerase chain reaction (RT-PCR) and antibody detection via enzyme-linked immunosorbent assay (ELISA) can be used to diagnose NiV.(3)
There are currently no approved vaccines or specific drugs designed to cure or prevent the Nipah virus infection. The main treatment for those with severe NiV cases is supportive care. Human-to-human transmission in this context is a concern, especially for exposed healthcare workers. The only way to prevent infection and transmission is to employ effective education strategies about reducing the risk of exposure to NiV. As of July 2022, the National Institute of Allergy and Infectious Diseases (NIAID) launched an early-stage clinical trial for a NiV mRNA vaccine.(4) This is the first clinical trial using the NIAID’s Pandemic Preparedness Plan approach, which prioritizes research on prototype pathogens and viruses with pandemic potential.
The World Health Organization (WHO) is supporting at risk countries by offering guidance for preventing and managing outbreaks.(2) If feasible, all bats must be kept away from fresh fruit products and sap collection sites. When this is not feasible, stopping consumption of specific fruits or fruit sap altogether, or washing and peeling all fruits potentially contaminated with fruit bat urine or saliva is recommended. To reduce animal-to-human transmission, protective attire should be worn when handling sick animals and animal premises should be quarantined as soon as signs of infection are detected. WHO recommends avoiding close physical contact with NiV infected patients and washing hands often. The high fatality rate of the Nipah virus has garnered attention from WHO as a priority disease and there will likely be additional research needed to generate better treatments and prevention methods.
by Anna Klavins and Taylor Slouka
R&D Department
Hardy Diagnostics
Meet the author

SENIOR TECHNICAL SERVICES AND R&D MANAGER at HARDY DIAGNOSTICS
Anna Klavins, RAC-Devices, B.S Cellular and Molecular Biology
Anna Klavins is the Senior Technical Services and R&D Manager at Hardy Diagnostics where she oversees the Research and Development, Design and Development, Quality Control, Technical Support, and Performance Studies teams. She earned a Molecular and Cellular Biology B.S. degree from Cal Poly San Luis Obispo while playing for the Division I NCAA women’s tennis team. Since joining Hardy Diagnostics in mid-2016, she has authored sixteen FDA 510(k) submissions for class II microbiology in vitro diagnostic devices. She has published in the Journal of Clinical Microbiology and the Journal of AOAC INTERNATIONAL, as well as presents in vitro diagnostic device performance evaluation results annually at global scientific conferences such as ASM Microbe, the AOAC Annual Meeting, and the International Association of Food Protection annual meeting. She is an advisor to the Joint CLSI-EUCAST Working Group and has earned the RAC-Devices certification.







