Rising Incidence of XDR Shigella
CDC issues an alert...Super Shigella on the Rise

Bacteria of the genus Shigella are clinically-significant pathogens which may cause mild to severe illness. Shigella comprises four species which include Shigella sonnei, Shigella flexneri, Shigella boydii, and Shigella dysenteriae. These bacteria cause an infection coined shigellosis, which infect an estimated 450,000 people in the United States each year.(1)
Shigellosis is characterized by symptoms of abdominal pain, fever, tenesmus (A painfully urgent but ineffectual attempt to urinate or defecate) and diarrhea that may be bloody and/or prolonged.(2)
Shigella dysenteriae produces shiga toxin which may cause severe symptoms and can be deadly. However, in many cases, people will not exhibit any symptoms of Shigella infection. At this time, the mortality rate by shigellosis is considered low in the United States. There are an estimated 40 deaths in the United States per year citing shigellosis as the cause.(3)
Shigella bacteria are easily transmissible via the fecal-oral route through food, water, and sexual contact.
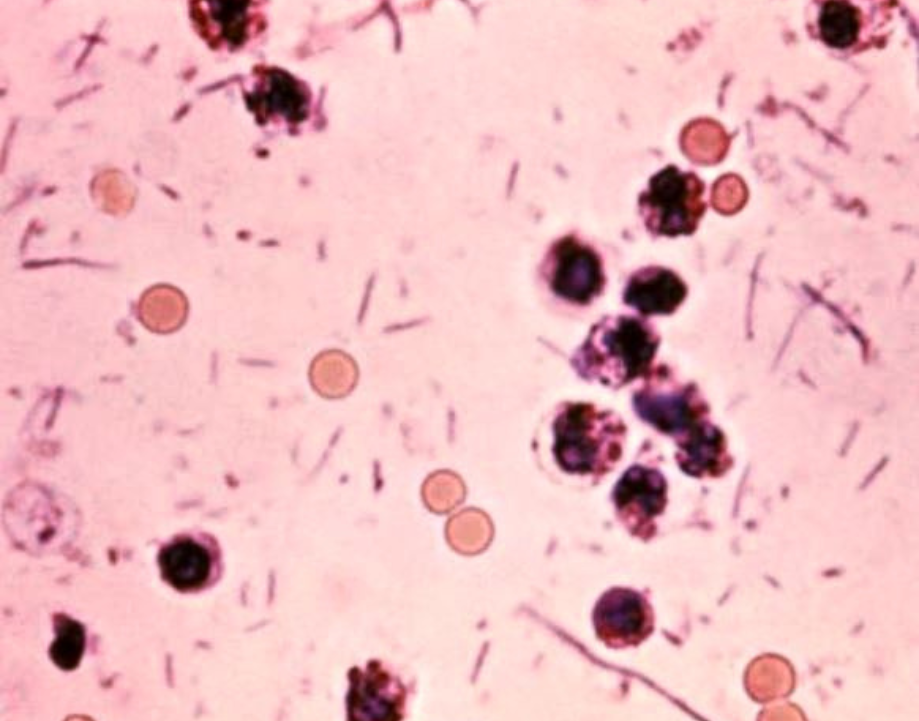
Shigella has an extremely low infectious dose of approximately 10-100 organisms. Young children, homeless people, travelers, those living with human immunodeficiency virus (HIV), as well as gay or bisexual men are most at risk for infection.(4) A photomicrograph of infected stool is shown below with the gram negative rods of Shigella and characteristic red blood cells.
Early this year, the CDC issued an urgent health advisory regarding XDR Shigella
In late February 2023, the Centers for Disease Control and Prevention (CDC) issued a health advisory due to an increase in cases of extensively drug-resistant (XDR) Shigella species.(4)
XDR Shigella are strains that are resistant to azithromycin, ciprofloxacin, ceftriaxone, trimethoprim-sulfamethoxazole, and ampicillin.
There are currently no CDC recommendations for treating XDR shigellosis. Alternate antibiotics are limited by US availability, lack of clinical data, as well as poor efficacy for infections in the gut lining.(5) The incidence of XDR Shigella infections has increased from 0% in 2015 to 5% in 2022. The National Antimicrobial Resistance Monitoring System (NARMS) serves to track XDR Shigella.(6)
An infection by Shigella is effectively diagnosed by stool culture on a culture medium such as HardyCHROM SS NoPRO Agar (shown above as teal colored colonies), or alternately, a PCR test. Antimicrobial susceptibility testing (AST) is ordered for positive stool cultures to guide antibiotic treatment for severe cases. Antibiotic treatment typically allows patients to recover faster, however, most people suffering from shigellosis will recover without antibiotic treatment within a week of infection.(1)
In order to reduce the chances of becoming infected with or transmitting Shigella, the CDC recommends: hand washing, avoiding food handling for others, staying home, not swimming, and abstaining from sex.
Written By: Trey Jensen - Technical Service Microbiologist at Hardy Diagnostics
Meet the author

TECHNICAL SERVICES MICROBIOLOGIST I at HARDY DIAGNOSTICS
Trey Jensen, B.S. Food Science & Technology
Trey is a Cal Poly Pomona graduate with a background in food safety and manufacturing. Trey is certified in Hazard Analysis Critical Control Point (HACCP). In his current role at Hardy Diagnostics, Trey provides technical product support and participates in AOAC International OMA program efforts for the development of food testing methods. In his free time, Trey enjoys family life with his wife, son, and daughter. In addition, Trey is a 3D design and printing enthusiast, avid gamer, and metal music enjoyer.